 Open Emergency Modal
Open Emergency Modal
 Open Emergency Modal
Open Emergency Modal
The Gastroenterology, Hepatology, and Endoscopy Department at Yashoda Super Speciality Hospital, Kaushambi, provides quaternary-level, multidisciplinary care for disorders of the digestive system, liver, pancreas, gallbladder, and bile ducts. With expertise in both adult and pediatric gastroenterology, our specialists manage everything from common conditions like acid reflux and irritable bowel syndrome to complex problems such as chronic liver disease, gastrointestinal cancers, inflammatory bowel disease, and metabolic liver disorders.
Equipped with advanced diagnostic suites, high-end ICUs, and minimally invasive endoscopic technology, the department ensures early detection, accurate diagnosis, and comprehensive treatment.
We provide 24×7 care for critical GI and liver emergencies where timely
intervention can be life-saving.
Common Emergencies Managed:
The hepatology division provides expert care for all liver conditions, ranging from hepatitis and fatty liver disease to cirrhosis and liver cancer. Using advanced imaging, FibroScan, liver biopsy, and molecular diagnostics, our hepatologists create personalized treatment plans. For patients with end-stage disease, liver transplantation is integrated as a life-saving therapy.
Conditions Treated:
Available Treatments And Procedures
Key Services:
Symptoms:
Jaundice, abdominal swelling,
unexplained weight loss, itching, fatigue, bleeding, and altered consciousness (encephalopathy).
This specialty addresses diseases of the bile ducts, gallbladder, and pancreas. From gallstones to pancreatic cancer, our biliary-pancreatic unit integrates advanced imaging, ERCP, EUS, and surgical interventions for precise and safe management.
Common Conditions:
Symptoms:
Severe upper abdominal pain
(radiating to back), jaundice, vomiting, fever with chills, unexplained weight loss, bloating, or loss of
appetite.
Our IBD unit specializes in long-term management of Crohn’s disease and ulcerative colitis. Patients are managed with a combination of biologics, immunotherapy, nutritional support, and surgical intervention when required.
Conditions Managed
Symptoms: Chronic diarrhea, rectal bleeding, weight loss, fatigue, abdominal cramps, joint pain, and skin rashes.
The GI oncology division is dedicated to cancers of the digestive tract, including the esophagus, stomach, pancreas, liver, colon, and rectum. Using a multimodal approach surgery, chemotherapy, radiation, targeted therapy, and immunotherapy we provide individualized treatment plans.
Common Cancers Treated:
Symptoms: Unexplained weight loss, blood in stool, abdominal pain, jaundice, persistent fatigue, loss of appetite.
This branch deals with diseases of the esophagus, stomach, intestines, and colon. It includes both functional disorders (like IBS) and structural/inflammatory conditions (like celiac disease and diverticulitis).
Conditions Managed
Symptoms: Heartburn, bloating, abdominal pain, nausea, diarrhea, constipation, difficulty swallowing.
Manometry testing evaluates the muscle activity of the digestive tract, helping diagnose swallowing, gastric emptying, and bowel movement disorders.
Conditions Diagnosed:
Why It Matters:
Our GI Surgery & HPB division provides advanced surgical solutions for cancers, benign conditions, and complex hepatobiliary disorders. Equipped with robotic platforms and high-definition laparoscopic systems, our surgeons perform precision procedures with minimal trauma and faster recovery.
Key Procedures:
Bariatric surgery is offered to patients with severe obesity and related comorbidities like type 2 diabetes, hypertension, and sleep apnea. Our approach focuses on long-term weight management and metabolic improvement using minimally invasive surgical options.
Procedures Performed:
These surgeries not only help patients achieve weight loss but also improve or resolve diabetes, fatty liver, hypertension, and metabolic syndrome.
Our Liver Transplant Program is designed for patients with end-stage liver disease and complex hepatology conditions. Transplants are performed by a dedicated team of hepatologists, surgeons, anesthetists, and transplant coordinators.
Indications:
Process:
The damaged liver is surgically
removed and replaced with a healthy liver from a deceased or living donor. Post-transplant care includes
immunosuppression, infection monitoring, and lifestyle modification to ensure long-term graft survival.
Benefits:

Director– GI - HBP Surgery, GI Oncology, Laparoscopic & Robotic Surgery and Liver Transplant.

Director - Gastroenterology, Hepatology & Endoscopy

Principal Consultant – Gastroenterology

A 28-year-old male from Nepal was diagnosed with chronic kidney disease after experiencing persistent weakness and loss of appetite for nearly two years. Investigations revealed severely impaired kidney function, and he was initiated on hemodialysis through a catheter placed in the right side of his neck. He was advised to undergo AV fistula creation and maintain regular maintenance hemodialysis (MHD) three times a week.
However, due to irregular dialysis sessions, his condition worsened. He then consulted the expert team of nephrologists, Dr. Prajit Mazumdar and Dr. Inderjit G. Momin, along with urologists, Dr. Vaibhav Sax...
A 28-year-old male from Nepal was diagnosed with chronic kidney disease after experiencing persistent weakness and loss of appetite for nearly two years. Investigations revealed severely impaired kidney function, and he was initiated on hemodialysis through a catheter placed in the right side of his neck. He was advised to undergo AV fistula creation and maintain regular maintenance hemodialysis (MHD) three times a week.
However, due to irregular dialysis sessions, his condition worsened. He then consulted the expert team of nephrologists, Dr. Prajit Mazumdar and Dr. Inderjit G. Momin, along with urologists, Dr. Vaibhav Saxena and Dr. Kuldeep Agarwal, at Yashoda Medicity. The team counselled him regarding renal replacement therapy (RRT), the importance of regular MHD, and recommended renal transplantation as the most effective long-term solution.
His transplant evaluation began with his mother as the donor. During the assessment, he was found to have significant anaemia and reduced cardiac function, likely resulting from inconsistent dialysis, which increased his peri-operative risk. After thorough counselling, he was optimised for surgery, and immunosuppressive therapy was initiated two days prior to the procedure.
The patient successfully underwent renal transplantation with ATG induction. Post-surgery, he showed excellent recovery with good urine output and steadily improving creatinine levels. He was discharged with a creatinine of 1.2 mg/dl and continues to do well on follow-up.
Treatment By:
Dr. Vaibhav Saxena, Dr. Kuldeep Agarwal, Dr. Prajit Mazumdar, and Dr. Inderjit G. Momin

Conquering a Complex Brain Aneurysm with Advanced Endovascular Therapy
A patient with a spinal condition was treated at Yashoda Medicity through a navigation-guided minimally invasive spine surgery, marking the first such procedure in the state. The surgery was performed in our state-of-the-art Neuro-Spine OT, equipped with O-arm, Stealth-8 Neuronavigation, Allen table, and IONM.
The procedure was led by Dr. Dibya Jyoti Mahakul, Consultant – Minimally Invasive Neuro-Spine Surgeon, who performed the surgery with unmatched precision. Using the neuronavigation system, the team could visualize the move...
Conquering a Complex Brain Aneurysm with Advanced Endovascular Therapy
A patient with a spinal condition was treated at Yashoda Medicity through a navigation-guided minimally invasive spine surgery, marking the first such procedure in the state. The surgery was performed in our state-of-the-art Neuro-Spine OT, equipped with O-arm, Stealth-8 Neuronavigation, Allen table, and IONM.
The procedure was led by Dr. Dibya Jyoti Mahakul, Consultant – Minimally Invasive Neuro-Spine Surgeon, who performed the surgery with unmatched precision. Using the neuronavigation system, the team could visualize the movements of all instruments in real time, ensuring the accurate placement of implants.
The minimally invasive approach resulted in minimal blood loss and muscle damage, and the patient experienced immediate pain relief. This achievement underscores our commitment to leveraging cutting-edge technology to provide safe, precise, and effective surgical solutions for spine problems.
At Yashoda Medicity, we care about your back. When it comes to spine conditions, you’re in safe hands.
Treatment By:
Dr. Dibya Jyoti Mahakul

First Navigation-Guided Minimally Invasive Spine Surgery at Yashoda Medicity
A patient with a spinal condition was treated at Yashoda Medicity through a navigation-guided minimally invasive spine surgery, marking the first such procedure in the state. The surgery was performed in our state-of-the-art Neuro-Spine OT, equipped with O-arm, Stealth-8 Neuronavigation, Allen table, and IONM.
The procedure was led by Dr. Dibya Jyoti Mahakul, Consultant – Minimally Invasive Neuro-Spine Surgeon, who performed the surgery with unmatched precision. Using the neuronavigation system, the team could visualize the mo...
First Navigation-Guided Minimally Invasive Spine Surgery at Yashoda Medicity
A patient with a spinal condition was treated at Yashoda Medicity through a navigation-guided minimally invasive spine surgery, marking the first such procedure in the state. The surgery was performed in our state-of-the-art Neuro-Spine OT, equipped with O-arm, Stealth-8 Neuronavigation, Allen table, and IONM.
The procedure was led by Dr. Dibya Jyoti Mahakul, Consultant – Minimally Invasive Neuro-Spine Surgeon, who performed the surgery with unmatched precision. Using the neuronavigation system, the team could visualize the movements of all instruments in real time, ensuring the accurate placement of implants.
The minimally invasive approach resulted in minimal blood loss and muscle damage, and the patient experienced immediate pain relief. This achievement underscores our commitment to leveraging cutting-edge technology to provide safe, precise, and effective surgical solutions for spine problems.
At Yashoda Medicity, we care about your back. When it comes to spine conditions, you’re in safe hands.
Treatment By:
Dr. Dibya Jyoti Mahakul

A 4-year-old, 11 kg child was brought to the Department of Pediatric Cardiac Sciences at Yashoda Medicity, Indirapuram, with complaints of bluish discoloration of fingernails and toes, poor weight gain, easy fatigue on walking, and recurrent hospital admissions.
Clinical evaluation revealed an oxygen saturation of 75%, prompting further investigations including echocardiography and CT pulmonary angiography.
The child was diagnosed with Cyanotic Congenital Heart Disease known as Tetralogy of Fallot (TOF), with additional apical muscular VSD and a hypoplastic pulmonary annulus.
The patient underwent open-heart surg...
A 4-year-old, 11 kg child was brought to the Department of Pediatric Cardiac Sciences at Yashoda Medicity, Indirapuram, with complaints of bluish discoloration of fingernails and toes, poor weight gain, easy fatigue on walking, and recurrent hospital admissions.
Clinical evaluation revealed an oxygen saturation of 75%, prompting further investigations including echocardiography and CT pulmonary angiography.
The child was diagnosed with Cyanotic Congenital Heart Disease known as Tetralogy of Fallot (TOF), with additional apical muscular VSD and a hypoplastic pulmonary annulus.
The patient underwent open-heart surgery called Intracardiac Repair, including closure of multiple VSDs with a transannular patch over the neopulmonary valve. The procedure was led by Dr. Abhinavsingh Chauhan, Consultant Pediatric Cardio-thoracic and Vascular Surgery. Advanced post-operative care in the Pediatric Cardiac ICU was uneventful, and post-operative echocardiography confirmed a successful repair.
The child was discharged in a stable and ambulatory condition on the 5th post-operative day, with oxygen saturation improving to 99%. This case reflects Yashoda Medicity’s expertise in managing complex pediatric cardiac conditions, combining cutting-edge surgical techniques with specialized intensive care to ensure safe, life-transforming outcomes for children.
Treatment By:
Dr. Abhinavsingh Chauhan

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert tea...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert team of doctors-Dr Prajit Mazumdar, Dr Inderjit G Momin,Dr Vaibhav Saxena and Dr Kuldeep Agarwal at Yashoda superspeciality Hospital, Kausambi who advised her to under renal transplant as it is the best form of renal replacement therapy. His Transplant workup was subsequently started and donor was wife and blood group was same.
However on transplant work up, it was found that he had Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% which increased his peri operative risk. Subsequently he was started on medicines and decongestion was done with diuretics and intensive hemodialysis. Subsequently renal transplantation was done after obtaining cardiology clearance with moderate risk and explaining the risk.
He underwent renal transplantation with Solumedrol and ATG induction. After transplantation he had good urine output with decreasing creatinine and was subsequently discharged with creatinine of 1.2 mg/dl . After transplant his pulmonary hypertension decreased and mitral regurgitation decreased which proves renal replacement therapy in form of transplant leads to improvement of cardiac condition. He is doing well on OPD follow up even today, 1.5 year after transplant with stable graft function and enjoying his life in myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A 4-year-old male child with congenital Pelvi-Ureteric Junction (PUJ) Obstruction underwent Robot-Assisted Pyeloplasty at Yashoda Medicity. The child had an excellent postoperative recovery and was discharged on postoperative day 2.
Robotic surgery offers superior precision and control, providing a significant advantage not only in cancer surgeries but also in pediatric minimally invasive procedures.
The benefits of robotic surgery over conventional techniques include smaller incisions, minimal intraoperative blood loss, enhanced surgical precision and dissection, reduced postoperative pain, and faster recovery and di...
A 4-year-old male child with congenital Pelvi-Ureteric Junction (PUJ) Obstruction underwent Robot-Assisted Pyeloplasty at Yashoda Medicity. The child had an excellent postoperative recovery and was discharged on postoperative day 2.
Robotic surgery offers superior precision and control, providing a significant advantage not only in cancer surgeries but also in pediatric minimally invasive procedures.
The benefits of robotic surgery over conventional techniques include smaller incisions, minimal intraoperative blood loss, enhanced surgical precision and dissection, reduced postoperative pain, and faster recovery and discharge.
The Department of Urology at Yashoda Medicity is committed to providing the highest standard of care to every patient, with special expertise in Robotic Surgery, Reconstructive Urology, Uro-Oncology, Stone Diseases, and Renal Transplant Surgeries.
Treatment By:
Dr. Vaibhav Saxena
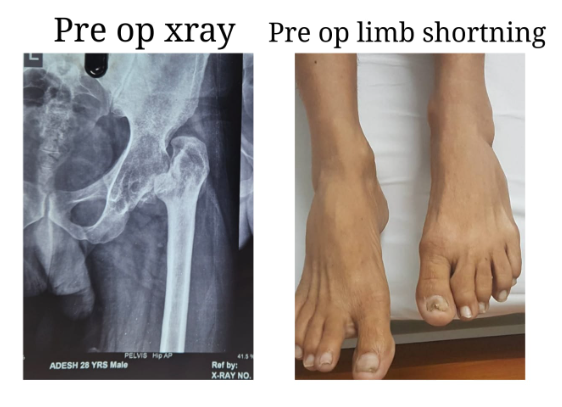
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting i...
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting in long-term sequelae.
This was a challenging case due to the chronic arthritic hip and associated soft tissue contractures. We performed an uncemented total hip replacement with subtrochanteric osteotomy. The procedure proceeded as planned: the limb length discrepancy was corrected, and the patient was mobilized within 24 hours. He was discharged after four days, pain-free, and walking with support.
He is expected to achieve full weight-bearing and return to all activities of daily living within eight to ten weeks.
Treatment By:
Dr. Amit Sharma

A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recomme...
A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recommended renal transplantation as the most effective form of renal replacement therapy. Her transplant workup was initiated, with her mother considered as the first donor option.
However, her mother was found to have diabetes, her father had a cardiac condition, and her husband was not a compatible blood group. With limited donor options, her mother-in-law, who had a matching blood group, came forward to donate a kidney and save her daughter-in-law’s life.
After obtaining clearance from cardiology, pulmonology, gynaecology, and psychiatry, along with approval from the authorisation committee, the transplant was successfully carried out with ATG induction. Post-transplant, she maintained good urine output with steadily improving creatinine levels. She was discharged with a creatinine of 1.2 mg/dl. The donor also recovered well and continues to do fine.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doct...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doctors, including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. Renal transplantation was advised as the most effective form of renal replacement therapy. His transplant workup was initiated, and his wife, who had a matching blood group, volunteered to donate.
During the evaluation, he was found to have mitral regurgitation, pulmonary hypertension, and a reduced ejection fraction of 35 percent, which significantly increased his perioperative risk. He was started on medications, optimised with diuretics, and maintained on intensive haemodialysis for decongestion. After cardiology clearance and counselling regarding moderate surgical risk, renal transplantation was planned.
He successfully underwent renal transplantation with Solumedrol and ATG induction. Post-transplant, he maintained good urine output with steadily decreasing creatinine levels and was discharged with a creatinine of 1.2 mg/dl. His pulmonary hypertension and mitral regurgitation also improved, demonstrating the positive impact of renal transplantation on cardiac function.
He continues to do well on outpatient follow-up, one and a half years after transplant, with stable graft function, and is enjoying a healthy life in Myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was expla...
A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was explained in view of end-stage renal disease.
His transplant workup was initiated, with his father considered as the first donor. However, he was rejected due to diabetes. Donor evaluation of his mother was then undertaken, but her blood group was incompatible with the recipient. In view of ABO incompatibility, anti-A and anti-B titres were assessed and revealed a high anti-B titre.
After detailed counselling regarding prognosis, risks, and cost, the family opted to proceed with an ABO-incompatible renal transplant. Rituximab was administered two weeks prior to transplantation, and he was started on tacrolimus and mycophenolate mofetil. This was followed by two sessions of Glycosorb column treatment on days 12 and 14, after which his anti-B titre decreased to 1:2. He then underwent renal transplantation with Solumedrol and Simulect induction, with anti-B titres monitored every 12 hours.
Post-transplant, he maintained brisk urine output and his serum creatinine gradually declined. He was discharged with a creatinine of 1.2 mg/dl and continues to do well on follow-up.
Treatment By:
Dr Prajit Mazumdar

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

Conquering a Complex Brain Aneurysm with Advanced Endovascular Therapy
Brain aneurysms are often described as ticking time bombs—silent, unpredictable, and potentially life-threatening if left untreated. They pose one of the most complex challenges in modern neurosurgery, requiring both precision and cutting-edge technology for successful management.
A 60-year-old woman presented with multiple episodes of severe headache, prompting her to consult Dr. Sumantao Chaterjee (Neurologist). Given the persistence and pattern of her symptoms, a brain angiography was recommended and performed by Dr. ...
Conquering a Complex Brain Aneurysm with Advanced Endovascular Therapy
Brain aneurysms are often described as ticking time bombs—silent, unpredictable, and potentially life-threatening if left untreated. They pose one of the most complex challenges in modern neurosurgery, requiring both precision and cutting-edge technology for successful management.
A 60-year-old woman presented with multiple episodes of severe headache, prompting her to consult Dr. Sumantao Chaterjee (Neurologist). Given the persistence and pattern of her symptoms, a brain angiography was recommended and performed by Dr. Dibya Jyoti Mahakul (Endovascular Neurosurgeon).
The imaging revealed a complex brain aneurysm, one that demanded meticulous planning due to its size, shape, location, and blood flow dynamics. After careful evaluation, the patient was offered a scarless, minimally invasive endovascular treatment. A flow diverter stent was strategically placed across the neck of the aneurysm to divert blood flow away from the aneurysm sac, promoting healing and preventing rupture. While technically challenging, the procedure was greatly aided by our state-of-the-art biplanar cath lab, equipped with advanced imaging tools like Vaso CT, CBCT, and MAFA software. These technologies ensured maximum precision, safety, and speed for both the patient and surgical team. Remarkably, the patient was discharged the very next day in a stable condition—aneurysm secured, risk averted.
Today, she is back home with her family, free from the shadow of a life-threatening condition, and ready to embrace life on her own terms.
Treatment By:
Dr. Dibya Jyoti Mahakul, Dr. Sumantao Chaterjee

A 51-year-old lady with left arm pain more than neck pain of 10 years duration, with BMI 44 and a short neck nearly the chin touching the chest, was diagnosed with OPLL C3-6 with myelopathy and fixed kyphosis of 20°. MRI showed cord signal changes at C5, and CT confirmed OPLL C3 -6 with high probability of intradural mass ( double density sign). Conventional wisdom (K line, kyphosis, anterior pathology etc.) dictated towards an anterior surgery, but possibility of dural laceration (intradural OPLL mass), with potential for other complications (cord / trachea / esophageal compression by pseudomeningole, meningitis, spinal cord ...
A 51-year-old lady with left arm pain more than neck pain of 10 years duration, with BMI 44 and a short neck nearly the chin touching the chest, was diagnosed with OPLL C3-6 with myelopathy and fixed kyphosis of 20°. MRI showed cord signal changes at C5, and CT confirmed OPLL C3 -6 with high probability of intradural mass ( double density sign). Conventional wisdom (K line, kyphosis, anterior pathology etc.) dictated towards an anterior surgery, but possibility of dural laceration (intradural OPLL mass), with potential for other complications (cord / trachea / esophageal compression by pseudomeningole, meningitis, spinal cord hernia etc.) were discussed in detail and a decission was taken to decompress and fix from the posterior aspect. The pre-op CT angio showed B/L high-riding vertebral arteries, which precluded the C2 screw.
Per operatively, the patient was positioned prone with the head clamped and a posterior exposure done. LM screw entry points were made from C3-6, followed by grade 1 facet resection at C3-4, C4-5, and C5-6 bilaterally. Further lordosis was achieved with manipulation of the head with the head clamp and closing the osteotomy gaps. LM screws (C3-6), a laminar screw at C2, and a pedicle screw at T1 & 2 were inserted and connected with rods.
C3-6 laminectomy was done, and the surgical site was closed after bone graft mixed with vancomycin was applied laterally.
Postoperative x-ray showed adequate lordosis (approximately 10 degrees) attainment.
The patient reported complete pain relief in the left shoulder and arm postoperatively.
Treatment By:
Dr. Ankur Goswami

A tremendous job has been done by Dr. Amit Sharma. I met with an accident in which the ACL ligament of my left knee was completely torn. I met Dr. Amit Sharma then he analysed the situation and told us about the procedure and the time period to recover from the injury. He has performed a successful surgery. The good thing is the confidence that Dr. Amit Sharma has on his surgery that he didn’t put braces on the knee while other doctors put the braces on for a month and then started Physiotherapy which will take a longer time period to heal from the injury.
Dr. Amit Sharma has started the Physiotherapy from the very next day of the surgery and i was discharged in 2 days, and the Physiotherapy is undergoing at my home. It's the 10th day today and I have gained so much confidence in 10 days that I am recovering very fast and in a few weeks I will be able to walk without any support.
Thanks to Dr. Amit Sharma, he is really having magical hands, he is very kind in nature, in my regular visits all of my stress went away after talking to him.
Again Thank You so much Doctor
Treatment By:
Dr. Amit Sharma
Mr. Ajeet Kumar Verma from Yashoda Homecare provided satisfactory service of sample collection. Well behaved, humble & polite person
“I had really good experience with Yashoda Home Care, the sample collection was very hygienically taken and pain-free, hassle-free. Mr. Ajeet was the phlebotomist.”
Had a good experience with Ajeet Kumar Verma from Yashoda Home Care who supported me while I was looking for someone to dress my mom’s stitches. He is very professional and a caring person.
Great support and service by the Home care department. Everyone from Ms Niharika, Mr. Anoop to all the attendants including Mr. Natwar Pandey, Mr Inam and Mr. Ajit, all have been superbly supportive and helpful throughout. God bless you all and highly recommended.
Very good services in home care Yashoda hospital his ish
Caretaker Deepanshu and Jatin and Satish is very good caretaker I have never seen better care takers in my life.
And he is very polite behaviour and friend in nature
Yashoda hospital Kaushambi service is very good according other hospital and other home care services
The home care facility provided by the hospital is also good, the staff which was at home was cooperative.
Home care services are Good. Mr. सुनील Sajwan was cooperative and the केयर taker Mrs. Shushila's वर्क has been quite satisfactory.
Had a. Very good experience with Yashoda Homecare, Kaushambi. The staff was very cooperative with excellent on time services. I would like to give a special mention to Mr Sunil Sajwan (Sales) and Sushila ji (PCA) for their quick response and excellent services.
Fully satisfied Mr .Ajeet Kumar Verma service Yashoda home care . vry good
Was great to recieve the best homecare services from yashoda hospital and really impressed with Ms. Niharika's support at the initial phase followed by Mr. Natwar Pandey who was really supportive in taking care of my father basic daily needs.
Thanks for all the support
Dr. Manish Singhal is a highly knowledgeable and experienced doctor. When patients and their families panic on hearing a word like ‘cancer’, Dr. Manish explains everything with such logic, scientific clarity and warmth that their anxiety eases. He has provided excellent treatment for my son’s Burkitt lymphoma. Dr. Manish and his entire team are extremely caring and humble. The overall experience at Yashoda Medicity is very smooth and reassuring.
An Extraordinary Orthopedic Surgeon with Unmatched Expertise
Dr. Amit sharma sir is truly a lifesaver and an outstanding orthopedic specialist.
After my severe accident, my injuries were extensive, and I was in urgent need of expert care. Dr. Amit sharma sir’s incredible skill in assessing and treating my complex fractures and injuries not only saved my life but also set me on the path to a full recovery.
I read somewhere doctors are like God now I believe in that…….thanks 🙏 to Dr. Amit sharma sir who gave me second chances in life….thanks alot sir for everything….you made my treatment possible.
The precision with which you performed multiple procedures, ensuring that my bones, joints, and ligaments were repaired to perfection, was nothing short of miraculous.
You showed great compassion and understanding throughout my treatment you patiently explained each step of the process, made me feel confident in my recovery, and provided me with the best care I could have asked for. Today, I am able to move, walk, and live my life normal again thanks to Dr. Amit sharma sir’s expertise in orthopedic surgery.
Thanks for giving me second chance.
I recently visited Yashoda Medcity Indirapuram for a gynecology appointment, and my experience was excellent. The doctor was very polite, patient, and attentive, taking the time to listen to all my concerns and explain everything clearly. The staff was helpful, and the overall process—from registration to consultation—was smooth and well-organized.
I truly appreciate the professional and caring approach. Highly recommended!
Visited Yashoda Medcity hospital for the first time for consultation with Dr. Rahul Chauda for my father. He is extremely helpful and explains diagnosis and treatment properly to the patient and their attendant. Also Ms. Simran in OPD helped us and guided us well.
I had my sister’s surgery done at Yashoda Medcity under Dr. Pradeep Diwan, and I’m extremely satisfied with the overall experience. Dr. Diwan is highly skilled, patient, and explains everything clearly, which made me feel very comfortable and confident throughout the process.
The hospital staff was also very supportive — from admission to discharge, everything was handled smoothly. The cleanliness, timely care, and overall hospitality were truly commendable.
Highly recommend Yashoda Medcity and Dr. Pradeep Diwan for anyone looking for expert medical care and a positive hospital experience!
My mother, Veena Tandon, was admitted here with severe chest pain. Dr. Manish Aggarwal and his team handled the situation with great care and professionalism. From quick diagnosis with ECG, echo, and CT angiography to patiently explaining the treatment options, everything was managed very smoothly. The doctor’s expertise and compassionate approach gave us confidence during a stressful time. We are truly grateful for the timely care and support provided. Highly recommend Dr. Manish Aggarwal and the hospital for cardiac treatment.
I had an exceptionally positive experience with Dr. Sumanth Bollu. His expertise in surgical oncology is evident from the very first consultation. He explains every detail with remarkable clarity and patience, making sure the patient and family feel fully informed and reassured.
I must say services in this hospital is top notch. This hospital has very good ambience and nice environment. OPD staff in medicine OPD is very coordinative and supportive. Doctor Vinay Bhat is excellent in his field and treating their patients.
The best hospital with the most amazing doctors!
I had a wonderful experience throughout my pregnancy and delivery. Dr. Samreen Zehra is truly the best gynecologist I’ve ever met — she explained everything clearly and provided not just medical care, but also technical, moral, and emotional support at every step. I always felt I was in the safest and most caring hands.
I underwent a C-section performed by Dr. J. B. Sharma, who is among the top 2% of doctors worldwide. He is incredibly talented, kind, and cooperative. Despite some complications, my delivery was absolutely safe — all thanks to Dr. J. B. Sharma, Dr. Samreen Zehra, and the entire Yashoda Hospital team.
The hospital’s technology and facilities are top-notch, and the staff are extremely supportive and caring. Highly recommend Yashoda Hospital for maternity care — they truly make you feel safe and cared for. 💖
I had consultation with Dr. Ankur Goswami for spine surgery. I had a great and satisfying experience during my wife’s surgery. Hospital staff is very nice and all staff of hospital, especially front office coordinator of orthopedics Ms. Rashmi Chaudhary, is very helpful and cooperative with us before and after treatment.
I am indebted and grateful to Dr. Ankur Goswami who is very experienced.
Wishing all a very happy times always.
Brig Man Mohan Mishra (R)
Greater Noida
Finally successful operation of father disease Lipoma has been done. Thanks a lot to Dr. Asheesh, Dr. Govind and Dr. Arindam Mukherjee, Nurses along with all staff. Nice experience, overall I can say every service of this hospital is outstanding.
Our heartfelt thanks to the entire Hospital, especially Dr Aayush Goyal and his team who performed the CABG surgery on our patient (Sh Arvind Bhatia) with extremely satisfactory results. Personal attention given to our case by the hospital COO, Dr. Sunil Dagar and the total management and the hospital staff, who ensured we were given utmost priority in all respects during the course of the treatment. Special thanks to Dr Asit Khanna for his diagnosis and guidance. Last but not the least, the homecare services provided by the hospital were really good.
Excellent services
Outstanding Results
We wish all the best to the hospital and its team.
