 Open Emergency Modal
Open Emergency Modal
 Open Emergency Modal
Open Emergency Modal
The Yashoda Institute of Cancer Care at Yashoda Group of Hospitals is at the forefront of comprehensive cancer management, offering preventive, diagnostic, medical, surgical, and radiation oncology services under one roof.
Our team of highly experienced oncologists, surgeons, radiation specialists, and more in Ghaziabad works collaboratively to provide personalized, evidence-based treatment plans for each patient. We combine world-class expertise with advanced technologies such as precision radiation, targeted therapies, and minimally invasive surgical techniques.
From early cancer detection to advanced multimodality treatment, our approach is always patient-first, ensuring the highest standards of care, safety, and compassion.
Our facilities include modern oncology wards, day-care chemotherapy suites, precision radiation units, and advanced imaging systems to deliver outcomes that focus on survival, recovery, and quality of life.

Director & Head - Hematology, Hemato-Oncology And Bone Marrow Transplant (Adult & Pediatrics)

Director, Department of Medical Oncology

Senior Consultant Surgical Oncology

Senior Consultant - Hematology, Hemato-Oncology And Bone Marrow Transplant (Adult & Pediatrics)

Consultant, Orthopedics Oncology

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert tea...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert team of doctors-Dr Prajit Mazumdar, Dr Inderjit G Momin,Dr Vaibhav Saxena and Dr Kuldeep Agarwal at Yashoda superspeciality Hospital, Kausambi who advised her to under renal transplant as it is the best form of renal replacement therapy. His Transplant workup was subsequently started and donor was wife and blood group was same.
However on transplant work up, it was found that he had Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% which increased his peri operative risk. Subsequently he was started on medicines and decongestion was done with diuretics and intensive hemodialysis. Subsequently renal transplantation was done after obtaining cardiology clearance with moderate risk and explaining the risk.
He underwent renal transplantation with Solumedrol and ATG induction. After transplantation he had good urine output with decreasing creatinine and was subsequently discharged with creatinine of 1.2 mg/dl . After transplant his pulmonary hypertension decreased and mitral regurgitation decreased which proves renal replacement therapy in form of transplant leads to improvement of cardiac condition. He is doing well on OPD follow up even today, 1.5 year after transplant with stable graft function and enjoying his life in myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal
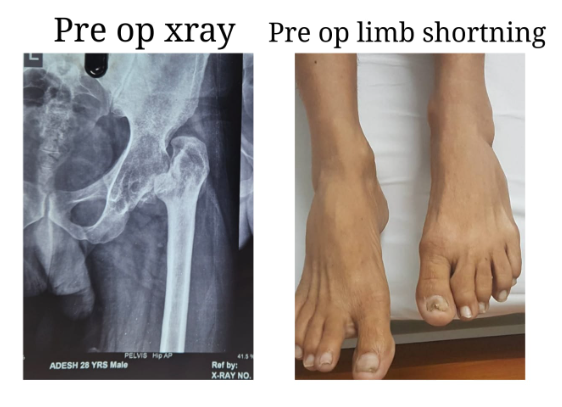
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting i...
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting in long-term sequelae.
This was a challenging case due to the chronic arthritic hip and associated soft tissue contractures. We performed an uncemented total hip replacement with subtrochanteric osteotomy. The procedure proceeded as planned: the limb length discrepancy was corrected, and the patient was mobilized within 24 hours. He was discharged after four days, pain-free, and walking with support.
He is expected to achieve full weight-bearing and return to all activities of daily living within eight to ten weeks.
Treatment By:
Dr. Amit Sharma

A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recomme...
A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recommended renal transplantation as the most effective form of renal replacement therapy. Her transplant workup was initiated, with her mother considered as the first donor option.
However, her mother was found to have diabetes, her father had a cardiac condition, and her husband was not a compatible blood group. With limited donor options, her mother-in-law, who had a matching blood group, came forward to donate a kidney and save her daughter-in-law’s life.
After obtaining clearance from cardiology, pulmonology, gynaecology, and psychiatry, along with approval from the authorisation committee, the transplant was successfully carried out with ATG induction. Post-transplant, she maintained good urine output with steadily improving creatinine levels. She was discharged with a creatinine of 1.2 mg/dl. The donor also recovered well and continues to do fine.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doct...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doctors, including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. Renal transplantation was advised as the most effective form of renal replacement therapy. His transplant workup was initiated, and his wife, who had a matching blood group, volunteered to donate.
During the evaluation, he was found to have mitral regurgitation, pulmonary hypertension, and a reduced ejection fraction of 35 percent, which significantly increased his perioperative risk. He was started on medications, optimised with diuretics, and maintained on intensive haemodialysis for decongestion. After cardiology clearance and counselling regarding moderate surgical risk, renal transplantation was planned.
He successfully underwent renal transplantation with Solumedrol and ATG induction. Post-transplant, he maintained good urine output with steadily decreasing creatinine levels and was discharged with a creatinine of 1.2 mg/dl. His pulmonary hypertension and mitral regurgitation also improved, demonstrating the positive impact of renal transplantation on cardiac function.
He continues to do well on outpatient follow-up, one and a half years after transplant, with stable graft function, and is enjoying a healthy life in Myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was expla...
A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was explained in view of end-stage renal disease.
His transplant workup was initiated, with his father considered as the first donor. However, he was rejected due to diabetes. Donor evaluation of his mother was then undertaken, but her blood group was incompatible with the recipient. In view of ABO incompatibility, anti-A and anti-B titres were assessed and revealed a high anti-B titre.
After detailed counselling regarding prognosis, risks, and cost, the family opted to proceed with an ABO-incompatible renal transplant. Rituximab was administered two weeks prior to transplantation, and he was started on tacrolimus and mycophenolate mofetil. This was followed by two sessions of Glycosorb column treatment on days 12 and 14, after which his anti-B titre decreased to 1:2. He then underwent renal transplantation with Solumedrol and Simulect induction, with anti-B titres monitored every 12 hours.
Post-transplant, he maintained brisk urine output and his serum creatinine gradually declined. He was discharged with a creatinine of 1.2 mg/dl and continues to do well on follow-up.
Treatment By:
Dr Prajit Mazumdar

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A tremendous job has been done by Dr. Amit Sharma. I met with an accident in which the ACL ligament of my left knee was completely torn. I met Dr. Amit Sharma then he analysed the situation and told us about the procedure and the time period to recover from the injury. He has performed a successful surgery. The good thing is the confidence that Dr. Amit Sharma has on his surgery that he didn’t put braces on the knee while other doctors put the braces on for a month and then started Physiotherapy which will take a longer time period to heal from the injury.
Dr. Amit Sharma has started the Physiotherapy from the very next day of the surgery and i was discharged in 2 days, and the Physiotherapy is undergoing at my home. It's the 10th day today and I have gained so much confidence in 10 days that I am recovering very fast and in a few weeks I will be able to walk without any support.
Thanks to Dr. Amit Sharma, he is really having magical hands, he is very kind in nature, in my regular visits all of my stress went away after talking to him.
Again Thank You so much Doctor
Treatment By:
Dr. Amit Sharma
Mr. Ajeet Kumar Verma from Yashoda Homecare provided satisfactory service of sample collection. Well behaved, humble & polite person
