 Open Emergency Modal
Open Emergency Modal
 Open Emergency Modal
Open Emergency Modal
Overview of Specialty
At Yashoda Medicity, we combine surgical excellence, cutting-edge technology, and compassionate care to treat the entire spectrum of heart, lung, and vascular conditions. Our department of cardiothoracic and vascular surgery delivers comprehensive, advanced surgical care from life-saving emergency procedures to minimally invasive and robotic innovations. Blending medical expertise with compassion, our team ensures that every patient gets the safest and most advanced treatment possible. Each service is designed to ensure the best possible outcome while focusing on patient comfort, safety, and quality of life.
Services Available
Adult Cardiac Surgery
Coronary Artery Bypass Grafting (CABG)
CABG restores blood supply to the heart by rerouting blood around blocked arteries. Durable grafts are selected based on individual anatomy, helping relieve chest pain, improve exercise capacity, and lower the risk of future heart attacks.
Beating Heart Bypass
In this advanced method, bypass is performed on the heart while it continues to beat, avoiding the use of a heart-lung machine. It is especially beneficial for elderly or high-risk individuals, with shorter recovery and fewer complications.
Total Arterial CABGBy using only arterial grafts, known for superior longevity, we maximize the lifespan of the bypass and minimize the chance of re-blockage. This approach is ideal for younger patients or those seeking the most durable solution. Total arterial CABG remains the gold standard treatment for patients with multivessel coronary artery disease.
Heart Valve Surgery
Valve Repairs
Whenever possible, the natural valve is repaired to maintain original tissue and function. This often leads to better long-term outcomes and reduces the need for lifelong blood-thinning medication.
Valve Replacements
When repair is not possible, valves are replaced with either mechanical or biological prostheses. This restores proper blood flow, relieves breathlessness or fatigue, and protects the heart and lungs from further strain.
Cardiac Tumors & RSOV Repairs
Cardiac tumors, though rare, can disrupt heart function or cause serious complications. We specialize in the surgical removal of benign and malignant heart tumors, as well as repairing ruptured sinus of Valsalva (RSOV), a critical defect where blood abnormally flows into the heart chambers. Early, precise surgery not only restores normal function but also prevents sudden deterioration.
Minimally Invasive Cardiac Surgery (MICS)
Minimally Invasive Bypass (MIDCAB) – Offers the benefits of traditional bypass surgery through small chest incisions, avoiding breastbone division. Patients recover faster with less pain and smaller scars.
Minimally Invasive Valve Replacements – Carried out through tiny incisions, providing the same effectiveness as open surgery but with shorter hospital stays and quicker return to routine.
Trans-Axillary Approaches – Innovative valve or ASD surgeries through an incision near the armpit. This reduces visible scarring and allows a faster, less painful recovery.
Pediatric Cardiac Surgery
Acyanotic CHD – ASD / VSD / PDA – We repair common congenital defects such as atrial septal defects, ventricular septal defects, and patent ductus arteriosus. Early correction ensures healthy growth, prevents strain on the heart and lungs, and allows children to lead active, healthy lives.
Cyanotic Conditions (TOF, TAPVC, Shunts) – For conditions where oxygen-poor blood circulates through the body, we perform corrective or palliative surgeries to restore oxygen levels. These interventions can dramatically improve a child’s energy, development, and survival.
Complex Congenital Defects – Advanced operations such as arterial switch or truncus repair offers children with life-threatening anomalies a chance at an active life.
Aortic Surgery
Dissections and Aneurysms – Dissections and aneurysms of the aorta are potentially life-threatening conditions that demand expert intervention. Our team performs both emergency and planned surgeries to repair the damaged vessel wall, replace affected segments with durable grafts, and prevent rupture or organ damage. Timely treatment can be the difference between a safe recovery and catastrophic complications.
Bentall’s Procedure – A complex operation replacing both the aortic valve and root in one operation. It is especially useful for patients with aneurysms, connective tissue disorders, or valve disease, ensuring a stable, long-lasting repair.
Hybrid Aortic Procedures – Combine open and minimally invasive approaches to handle complex cases safely, with quicker recovery.
Vascular Surgery
Vascular Surgery
Our vascular surgery programme provides complete care for conditions affecting arteries and veins across the body. From complex bypass operations to minimally invasive endovascular therapies, the focus is on restoring healthy blood flow, easing symptoms, and preventing limb-threatening complications. Every treatment is planned to suit individual needs.
Endovenous Laser Ablation (EVLA) for Varicose Veins
EVLA is a modern, walk-in procedure designed to treat painful or visible varicose veins. A fine catheter delivers laser energy to seal the affected vein, redirecting blood to healthier vessels. With almost no scarring, this technique offers quick relief from heaviness, swelling, and cramping in the legs, while allowing a fast return to normal activities.
Peripheral Vascular Procedures
These treatments target narrowing or blockages in the arteries that supply blood to the legs, arms, or other areas. Angioplasty, stenting, and bypass surgery are used to improve circulation, reduce discomfort, and restore mobility. Early treatment of peripheral artery disease also lowers the risk of ulcers, gangrene, or loss of limb.
Percutaneous Aortic & Vascular Interventions
TAVI (Transcatheter Aortic Valve Implantation)
This minimally invasive technique replaces diseased aortic valves without the need for open-heart surgery. A new valve is placed through a catheter, making it an effective choice for individuals at higher surgical risk, while delivering strong long-term outcomes.
EVAR & TEVAR
Endovascular Aneurysm Repair (EVAR) and Thoracic Endovascular Aneurysm Repair (TEVAR) involve placing stent grafts through small groin incisions to repair aneurysms. This method avoids large cuts, shortens recovery, and reduces post-procedure discomfort.
Hybrid Procedures
Hybrid approaches combine catheter-based techniques with open surgery in the same session. This method is particularly valuable for complex cases, offering the advantages of both strategies together.
Robotic-Assisted Cardiac Surgery
Robotics allow surgeons to work through small incisions with enhanced precision and control.
Robotic-Assisted CABG
Using robotic technology, we perform coronary bypasses through tiny incisions with unparalleled precision. Patients experience less pain, reduced blood loss, and a quicker return to normal activities without compromising surgical results.
Robotic Valve / ASD / Myxoma Surgery
Robotics allow delicate repairs or replacements of valves, closure of atrial septal defects, and removal of benign tumors with minimal trauma. Enhanced vision and instrument control mean shorter recovery times and better cosmetic outcomes.
Heart Failure & Advanced Therapies
ECMO – ECMO temporarily takes over the function of the heart and lungs, allowing them to rest and heal during severe illness or after major surgery. It is often a life-saving bridge to recovery or further treatment.
Ventricular Assist Devices (VADs) – Mechanical pumps that support heart function in patients with advanced heart failure. VADs can be used while waiting for a transplant or as long-term therapy for those who are not transplant candidates.
Heart Transplantation – For patients with end-stage heart disease, transplantation offers the chance of a longer, healthier life. We provide comprehensive care from evaluation and surgery to long-term follow-up.
Cardiovascular Emergencies
When seconds matter, our cardiac and vascular surgeons are equipped to handle the most critical emergencies, be it massive heart attacks or a major vessel injuries. A 24×7 surgical response, backed by advanced imaging, hybrid operating rooms, and critical care support, ensures that patients get life-saving treatment without delay.
Ventricular Septal Ruptures
A serious complication of severe heart attacks, a ventricular septal rupture creates a dangerous hole between the heart’s pumping chambers. Surgical repair involves patching the defect and stabilizing heart function, preventing rapid decline and restoring effective circulation.
Aortic Dissections
An aortic dissection occurs when a tear develops in the inner wall of the aorta, allowing blood to flow between the layers of the vessel wall. This is a true surgical emergency. Our team performs immediate repairs to replace or reinforce the damaged section, stopping the dissection’s progression and preserving life.
Cardiac Trauma
Penetrating injuries (such as stab wounds) or blunt force trauma (such as car accidents) to the heart require urgent, specialized care. Our surgeons perform rapid repair of heart muscle, valves, and vessels to control bleeding, restore function, and prevent fatal complications.
Conditions Treated
 More
More

Senior Consultant, Cardiothoracic & Vascular Surgery

Consultant Cardiothoracic Surgery

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert tea...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% underwent successful transplant
A middle aged male was diagnosed with chronic kidney disease when he developed generalized body weakness, puffiness of face and swelling of legs with nausea, intermittent vomiting . On Investigations, he was found to have deranged renal function with urea-300 mg/dl,creatinine of 15 mg/dl, hb-9 mg and was subsequently started on hemodialysis via catheter inserted in right side of neck.
He subsequently visited India where he consulted our expert team of doctors-Dr Prajit Mazumdar, Dr Inderjit G Momin,Dr Vaibhav Saxena and Dr Kuldeep Agarwal at Yashoda superspeciality Hospital, Kausambi who advised her to under renal transplant as it is the best form of renal replacement therapy. His Transplant workup was subsequently started and donor was wife and blood group was same.
However on transplant work up, it was found that he had Mitral Regurgitation, pulmonary hypertension and low ejection fraction-35% which increased his peri operative risk. Subsequently he was started on medicines and decongestion was done with diuretics and intensive hemodialysis. Subsequently renal transplantation was done after obtaining cardiology clearance with moderate risk and explaining the risk.
He underwent renal transplantation with Solumedrol and ATG induction. After transplantation he had good urine output with decreasing creatinine and was subsequently discharged with creatinine of 1.2 mg/dl . After transplant his pulmonary hypertension decreased and mitral regurgitation decreased which proves renal replacement therapy in form of transplant leads to improvement of cardiac condition. He is doing well on OPD follow up even today, 1.5 year after transplant with stable graft function and enjoying his life in myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal
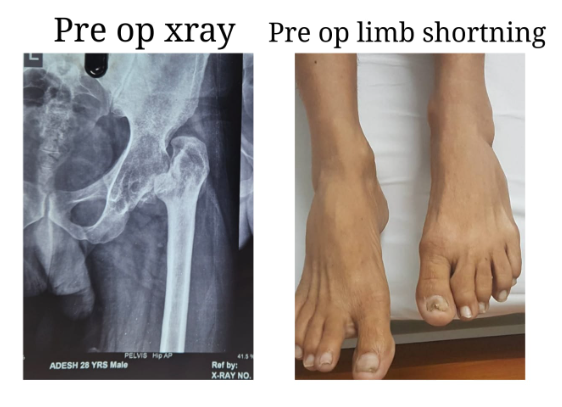
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting i...
Total Hip Replacement in a Young Adult with Secondary Osteoarthritis of the Hip due to Sequelae of Childhood Septic Arthritis
Early and effective treatment of childhood hip septic arthritis is crucial to prevent or minimize long-term complications such as avascular necrosis, hip dislocation, osteoarthritis, and leg length discrepancy.
We present a case of a 30-year-old male patient suffering from secondary osteoarthritis of the left hip, with complete destruction of the joint over the past 20 years. He had septic arthritis of the left hip at the age of 9, which was only partially treated, resulting in long-term sequelae.
This was a challenging case due to the chronic arthritic hip and associated soft tissue contractures. We performed an uncemented total hip replacement with subtrochanteric osteotomy. The procedure proceeded as planned: the limb length discrepancy was corrected, and the patient was mobilized within 24 hours. He was discharged after four days, pain-free, and walking with support.
He is expected to achieve full weight-bearing and return to all activities of daily living within eight to ten weeks.
Treatment By:
Dr. Amit Sharma

A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recomme...
A new life donated to daughter-in law by mother in law
A 30-year-old female was diagnosed with chronic kidney disease after presenting with generalised weakness, loss of appetite, and intermittent vomiting. Investigations revealed impaired renal function, and she was started on haemodialysis through a catheter placed in the right side of her neck. She was advised maintenance haemodialysis three times a week.
She consulted our expert team of doctors including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. They recommended renal transplantation as the most effective form of renal replacement therapy. Her transplant workup was initiated, with her mother considered as the first donor option.
However, her mother was found to have diabetes, her father had a cardiac condition, and her husband was not a compatible blood group. With limited donor options, her mother-in-law, who had a matching blood group, came forward to donate a kidney and save her daughter-in-law’s life.
After obtaining clearance from cardiology, pulmonology, gynaecology, and psychiatry, along with approval from the authorisation committee, the transplant was successfully carried out with ATG induction. Post-transplant, she maintained good urine output with steadily improving creatinine levels. She was discharged with a creatinine of 1.2 mg/dl. The donor also recovered well and continues to do fine.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doct...
An International patient from Myanmar with Mitral Regurgitation, pulmonary hypertension, and low ejection fraction-35% underwent successful transplant
A middle-aged male was diagnosed with chronic kidney disease after developing generalised weakness, facial puffiness, swelling of the legs, nausea, and intermittent vomiting. Investigations revealed severely impaired renal function with urea of 300 mg/dl, creatinine of 15 mg/dl, and haemoglobin of 9 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck.
He later visited India and consulted our expert team of doctors, including Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal at Yashoda Superspeciality Hospital, Kaushambi. Renal transplantation was advised as the most effective form of renal replacement therapy. His transplant workup was initiated, and his wife, who had a matching blood group, volunteered to donate.
During the evaluation, he was found to have mitral regurgitation, pulmonary hypertension, and a reduced ejection fraction of 35 percent, which significantly increased his perioperative risk. He was started on medications, optimised with diuretics, and maintained on intensive haemodialysis for decongestion. After cardiology clearance and counselling regarding moderate surgical risk, renal transplantation was planned.
He successfully underwent renal transplantation with Solumedrol and ATG induction. Post-transplant, he maintained good urine output with steadily decreasing creatinine levels and was discharged with a creatinine of 1.2 mg/dl. His pulmonary hypertension and mitral regurgitation also improved, demonstrating the positive impact of renal transplantation on cardiac function.
He continues to do well on outpatient follow-up, one and a half years after transplant, with stable graft function, and is enjoying a healthy life in Myanmar.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was expla...
A case of ABO incompatible transplant with high ANTI B TITRES
A 37-year-old male was diagnosed with chronic kidney disease three years ago after presenting with frothy urine and hypertension. Initial investigations revealed a serum creatinine of 3 mg/dl. Over the next few years, his kidney function deteriorated, and he was started on maintenance haemodialysis three times a week via an arteriovenous fistula. He was referred to our hospital by a former recipient who had undergone renal transplantation under Dr Prajit Mazumdar. On evaluation by our team of doctors, the need for renal transplantation was explained in view of end-stage renal disease.
His transplant workup was initiated, with his father considered as the first donor. However, he was rejected due to diabetes. Donor evaluation of his mother was then undertaken, but her blood group was incompatible with the recipient. In view of ABO incompatibility, anti-A and anti-B titres were assessed and revealed a high anti-B titre.
After detailed counselling regarding prognosis, risks, and cost, the family opted to proceed with an ABO-incompatible renal transplant. Rituximab was administered two weeks prior to transplantation, and he was started on tacrolimus and mycophenolate mofetil. This was followed by two sessions of Glycosorb column treatment on days 12 and 14, after which his anti-B titre decreased to 1:2. He then underwent renal transplantation with Solumedrol and Simulect induction, with anti-B titres monitored every 12 hours.
Post-transplant, he maintained brisk urine output and his serum creatinine gradually declined. He was discharged with a creatinine of 1.2 mg/dl and continues to do well on follow-up.
Treatment By:
Dr Prajit Mazumdar

A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more...
A challenging Case of renal transplant with a history of >22 units of blood transfusion and class 1 DSA positive
A 26-year-old male was diagnosed with chronic kidney disease after developing generalised weakness and loss of appetite. Investigations revealed impaired renal function with a creatinine of 12 mg/dl and haemoglobin of 5 g/dl. He was started on haemodialysis through a catheter placed in the right side of his neck and advised AV fistula creation with maintenance haemodialysis three times a week.
Despite regular dialysis, his anaemia persisted and he required multiple blood transfusions (more than 22 units over three months) even while receiving erythropoietin and iron therapy. Anaemia workup revealed occult blood in the stool, and upper GI endoscopy confirmed peptic ulcer disease.
He consulted our team of nephrologists (Dr Prajit Mazumdar and Dr Inderjit G. Momin) and urologists (Dr Vaibhav Saxena and Dr Kuldeep Agarwal) at Yashoda Superspeciality Hospitals, Kaushambi, where renal transplantation was advised. His mother, who had a matching blood group, was identified as the donor. However, transplant workup revealed donor-specific antibodies on single antigen bead testing (Class I) with an MFI greater than 2500 on multiple beads, most likely due to the multiple blood transfusions. This significantly increased the risk of acute rejection in the immediate post-transplant period, making the case high-risk.
After thorough counselling regarding risks, he underwent desensitisation with two sessions of plasmapheresis and IVIg to reduce the donor-specific antibodies. He then successfully underwent renal transplantation with ATG induction. Post-transplant, he maintained good urine output with steadily improving creatinine levels and was discharged with a creatinine of 1.2 mg/dl.
He continues to do well on outpatient follow-up.
Treatment By:
Dr Prajit Mazumdar, Dr Inderjit G. Momin, Dr Vaibhav Saxena, and Dr Kuldeep Agarwal

A tremendous job has been done by Dr. Amit Sharma. I met with an accident in which the ACL ligament of my left knee was completely torn. I met Dr. Amit Sharma then he analysed the situation and told us about the procedure and the time period to recover from the injury. He has performed a successful surgery. The good thing is the confidence that Dr. Amit Sharma has on his surgery that he didn’t put braces on the knee while other doctors put the braces on for a month and then started Physiotherapy which will take a longer time period to heal from the injury.
Dr. Amit Sharma has started the Physiotherapy from the very next day of the surgery and i was discharged in 2 days, and the Physiotherapy is undergoing at my home. It's the 10th day today and I have gained so much confidence in 10 days that I am recovering very fast and in a few weeks I will be able to walk without any support.
Thanks to Dr. Amit Sharma, he is really having magical hands, he is very kind in nature, in my regular visits all of my stress went away after talking to him.
Again Thank You so much Doctor
Treatment By:
Dr. Amit Sharma
Mr. Ajeet Kumar Verma from Yashoda Homecare provided satisfactory service of sample collection. Well behaved, humble & polite person
“I had really good experience with Yashoda Home Care, the sample collection was very hygienically taken and pain-free, hassle-free. Mr. Ajeet was the phlebotomist.”
Had a good experience with Ajeet Kumar Verma from Yashoda Home Care who supported me while I was looking for someone to dress my mom’s stitches. He is very professional and a caring person.
Great support and service by the Home care department. Everyone from Ms Niharika, Mr. Anoop to all the attendants including Mr. Natwar Pandey, Mr Inam and Mr. Ajit, all have been superbly supportive and helpful throughout. God bless you all and highly recommended.
Very good services in home care Yashoda hospital his ish
Caretaker Deepanshu and Jatin and Satish is very good caretaker I have never seen better care takers in my life.
And he is very polite behaviour and friend in nature
Yashoda hospital Kaushambi service is very good according other hospital and other home care services
The home care facility provided by the hospital is also good, the staff which was at home was cooperative.
Home care services are Good. Mr. सुनील Sajwan was cooperative and the केयर taker Mrs. Shushila's वर्क has been quite satisfactory.
Had a. Very good experience with Yashoda Homecare, Kaushambi. The staff was very cooperative with excellent on time services. I would like to give a special mention to Mr Sunil Sajwan (Sales) and Sushila ji (PCA) for their quick response and excellent services.
Fully satisfied Mr .Ajeet Kumar Verma service Yashoda home care . vry good
Was great to recieve the best homecare services from yashoda hospital and really impressed with Ms. Niharika's support at the initial phase followed by Mr. Natwar Pandey who was really supportive in taking care of my father basic daily needs.
Thanks for all the support
